Zaven Sargsyan@sargsyanz
Aug 1, 2019
14 tweets
Orthostatic hypotension and vitals: short #tweetorial with a case, couple principles, and a few tips.
Here’s the case: A lady, 70, got up to take her plate to the sink, got dizzy, and fell. She often gets dizzy with standing, but it usually passes in a few seconds.
1/13
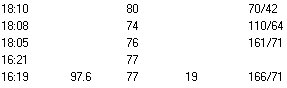
Check out her vitals below, esp top 3 rows:
- what do you think of their timing?
- what positioning do you think was used for each set?
- anything surprise you about the values?
- can you draw any conclusions about the *cause* of orthostasis in this case?
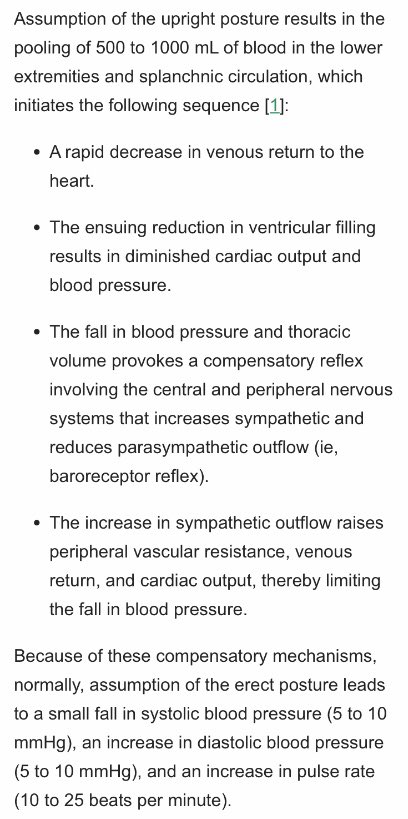
Normal physiology: When we stand up, 0.5-1L of venous blood gets pulled  by gravity. Sympathetics (norepinephrine) quickly compensate: alpha-1 squeezes blood vessels to
by gravity. Sympathetics (norepinephrine) quickly compensate: alpha-1 squeezes blood vessels to  venous return, beta-1 makes heart beat faster and harder.
Few more details from @UpToDate if interested:
venous return, beta-1 makes heart beat faster and harder.
Few more details from @UpToDate if interested:
 by gravity. Sympathetics (norepinephrine) quickly compensate: alpha-1 squeezes blood vessels to
by gravity. Sympathetics (norepinephrine) quickly compensate: alpha-1 squeezes blood vessels to  venous return, beta-1 makes heart beat faster and harder.
Few more details from @UpToDate if interested:
venous return, beta-1 makes heart beat faster and harder.
Few more details from @UpToDate if interested: If compensation fails (BP drops >20/10), either the reflex didn’t work right, or there is such a situation that despite full function, the compensation wasn’t enough.
How can we distinguish?
Tip 1: Interpret the heart rate.
If BP falls but HR  , orthostasis is more likely from autonomic dysfunction.
If BP falls and HR
, orthostasis is more likely from autonomic dysfunction.
If BP falls and HR  , more likely low preload or highly preload-dependent state.
, more likely low preload or highly preload-dependent state.
 , orthostasis is more likely from autonomic dysfunction.
If BP falls and HR
, orthostasis is more likely from autonomic dysfunction.
If BP falls and HR  , more likely low preload or highly preload-dependent state.
, more likely low preload or highly preload-dependent state.I say “low preload” rather than hypovolemia to help us think beyond dehydration and bleeding. For example, sepsis is a common cause of orthostatic hypotension. Before vasodilation and third-spacing progress enough to cause supine hypotension, you’re orthostatic.
Tip 2: It’s quicker for you to check orthostatics yourself than to
(a) request them
(b) make a note to follow up on the results
(c) follow up on the results
(d) need to clarify technique, whether concurrent symptoms, etc
Ok, so how do we do it?
Tip 3: Take the first measurement within 1 minute.
Remember our lady? She gets lightheaded right after standing, and it passes in seconds. I bet you’ve felt this too.
If you wait 3 min, you’ll miss the hypotension.
@AlbertoPuig6 wrote about this in @SGIM Forum:
Delayed orthostasis can happen too, so do repeat standing VS a couple min later.
Oh, and skip the sitting measurement. It doesn’t really add much.
Here is a great one-page guide from the CDC on how to check orthostatics.
bit.ly/2yrHVlX
Tip 4: Always consider impact of meds.
They can cause orthostasis themselves, but can also mess with rules of thumb in Tip 1 when layered over another process.
E.g. with BBL, HR might  even if low preload. By contrast, alpha-blocker could
even if low preload. By contrast, alpha-blocker could  BP with
BP with  HR.
HR.
 even if low preload. By contrast, alpha-blocker could
even if low preload. By contrast, alpha-blocker could  BP with
BP with  HR.
HR.Tip 5: Realize limitations of this (and any) test.
Baseline orthostatic hypotension is prevalent in elderly, on order of 20% or more, and is often asymptomatic/ inconsequential.
bit.ly/2WVu2GF
bit.ly/2xaWLwA
Test could be + but unrelated to why you checked.
Back to our case. She had diabetes and bad peripheral neuropathy (similar ddx to autonomic neuropathy). She had been having chills and dysuria a few days. Symptoms improved with fluids/antibiotics. Orthosratic BP drop improved but didn’t resolve.
Summary: tips on orthostatic vitals/hypoTN:
- skip the sitting and check the first standing BP within 1 min
- BP  and HR
and HR  supports low-preload. HR
supports low-preload. HR  supports autonomic failure.
- meds can cause orthostasis or confound VS pattern
- orthostasis often an incidental/asx finding
supports autonomic failure.
- meds can cause orthostasis or confound VS pattern
- orthostasis often an incidental/asx finding
 and HR
and HR  supports low-preload. HR
supports low-preload. HR  supports autonomic failure.
- meds can cause orthostasis or confound VS pattern
- orthostasis often an incidental/asx finding
supports autonomic failure.
- meds can cause orthostasis or confound VS pattern
- orthostasis often an incidental/asx findingThanks for reading!

Zaven Sargsyan
@sargsyanz
Internist at Baylor College of Medicine. Alum @BCMHouston and @MGHMedicine. Tweets about medicine and language. Opinions my own.
Missing some tweets in this thread? Or failed to load images or videos? You can try to .