Eric Jaeger, JD, NRP, EMS IC (He/Him)@EricJaegerTNG
Nov 25, 2022
20 tweets
The Lazarus Phenomenon: When the Dead Awaken
A thread...  Like Lazarus in Bible, there are well documented case reports of patients spontaneously “coming back to life” after resuscitation has been terminated.
Like Lazarus in Bible, there are well documented case reports of patients spontaneously “coming back to life” after resuscitation has been terminated.
 Like Lazarus in Bible, there are well documented case reports of patients spontaneously “coming back to life” after resuscitation has been terminated.
Like Lazarus in Bible, there are well documented case reports of patients spontaneously “coming back to life” after resuscitation has been terminated. Lazarus Phenomenon TLDR:
- Occurs surprisingly often; many well documented case reports
- Neuro intact survival NOT uncommon!
- Causation not well understood
- Negligence? Occasionally...
- Causes incl hyperinflation, pseudo-PEA, hypothermia, delayed med effect, OMI reperfusion
Take Home Points:
- Check for factors interfering w/ ROSC: low temp, auto-PEEP, hypoglycemia, low flow
- Be hesitant to terminate w/ VF & PEA
- Stop using time to decide futility
- Prolonged resus is often warranted
- Be careful with ventilations
- Observe post-termination
"Autoresuscitation" is the medical term for the phenomenon.
It occurs surprisingly often. There are many well documented case reports of pts who have come back to life after being declared dead.
1/3 - 1/2 of surveyed physicians report having seen it.
link.springer.com/article/10.118
How much time may pass before the pt awakens?
While often brief (<5 mins), there are multiple cases of apparently deceased pts awakening after 20 mins or longer!
In one case series:
- 50% < 5 mins
- 75% < 10 mins
- 25% 10+ mins
Remarkably, up to 1/3 of survivors are discharged neurologically intact.
Anoxic brain injury is the primary enemy of those who ultimately succumb.
What causes the phenomenon?
Some cases are due to negligence, but in other cases the explanation is less clear.
dailymail.co.uk/news/article-8
Likely causes include:
- Iatrogenic hyperinflation
- Pseudo-PEA
- Hypothermia
- Delayed med effect
- Spontaneously reperfusing OMI
- Non-Asystole rhythms that self resolve
- Transient asystole after defibrillation
Iatrogenic hyperinflation occurs when ventilation is too vigorous, causing overinflation of the lungs and/or abdomen. The resulting increase in intrathoracic pressure is thought to impede blood return to the heart.
pubmed.ncbi.nlm.nih.gov/21378522/
Pseudo-PEA is a profound shock state in which the pt appears to be in cardiac arrest but has an organized cardiac rhythm and a weak pulse that is undetectable by palpation.
emergencymedicinecases.com/pea-arrest-pse
Hypothermia is well known to interfere with defibrillation & may slow the effectiveness of resus meds. Occult hypothermia is not uncommon. The AHA notes that patients may need to be rewarmed to over 30°C (86°F) before defibrillation is successful.
ahajournals.org/doi/10.1161/ci
Take Home Points
#1 Use Final Minutes of Resus Wisely
For the LOVE OF GOD stop giving sodium bicarb at the end!
Instead look for factors interfering with ROSC:
Temp<90°F? >Continue CPR & rewarm
Hyperinflation? >Disconnect BVM
Ultrasound? >Check for low flow
Blood Glucose? >D10
#2 Be Careful Stopping with PEA or VFib
(or anything other than Asystole)
Be cautious in the presence of a rhythm that is potentially treatable or compatible with life. Decision to stop must be based on unequivocal clinical evidence of death.
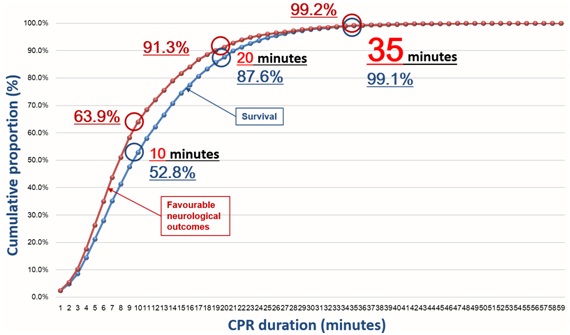
#3 Stop Watching the Clock
It is a myth that resuscitation after 20 mins is usually futile.
Many pts survive neurologically intact with resus > 20 mins. Stop using time as a basis for whether to stop resuscitation. Instead use the relevant medical factors to drive the decision.
Factors relevant to determining futility:
- Witnessed vs. Unwitnessed
- Bystander CPR vs. No CPR
- Asystole vs. Shockable Rhythm
- EtCO2
- Multiple comorbidities/Frail vs. Healthy
- Cardiac activity on POCUS
#4 Prolonged resuscitation is often warranted:
- Hypothermic cardiac arrest
- Narrow complex PEA
- Recurrent/refractory VF/VT
- Reversible cause (PE, tamponade, hemorrhage)
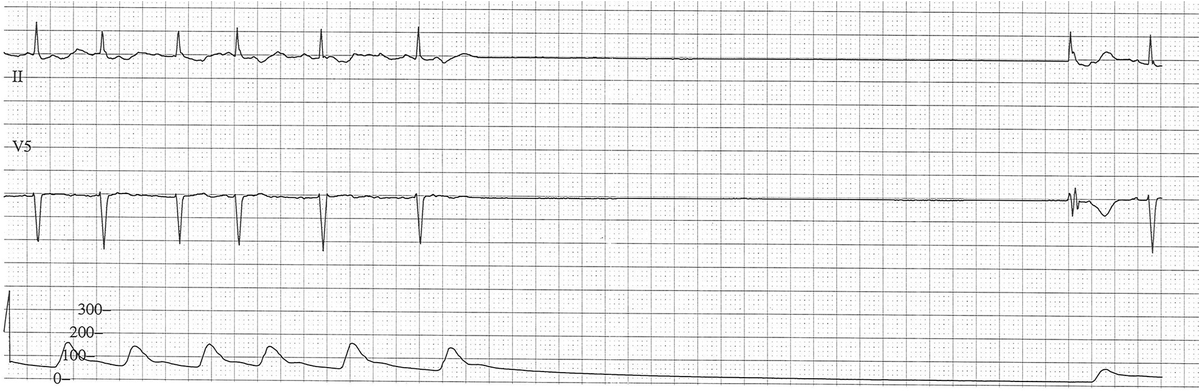
#5 Confirm Asystole
Observe long enough to ensure that apparent asystole is not transient and not severe bradycardia. Transient asystole following defibrillation is not uncommon.
#6 Traumatic Cardiac Arrest is Final
Almost all case reports of autoresuscitation involve a medical etiology for cardiac arrest. Overall, survival from traumatic cardiac arrest is rare, and there are exceedingly few cases of autoresuscitation following TCA.
#7 Avoid Over Ventilation
Avoid over ventilating patients in cardiac arrest. High intrathoracic pressure and hyperinflation may be a frequent cause of autoresuscitation. Use two fingers or one-hand or a pediatric BVM. Squeeze gently. Allow adequate time for exhalation.
#8 Post-Termination Observation
Just in case...
Guidelines recommend observing the pt for 5-10 mins post-termination.
/End

Eric Jaeger, JD, NRP, EMS IC (He/Him)
@EricJaegerTNG
Focused on EMS leadership, protocol development, education and system oversight. RSI Paramedic/Educator in the ED & in the field. Evidence-based medicine!
Missing some tweets in this thread? Or failed to load images or videos? You can try to .